Children's National celebrates Valentine's Day with Dr. Bear Bot, a new robot in the cardiac intensive care unit

WASHINGTON — A new robot who lives in the cardiac intensive care unit (cardiac ICU) at Children’s National Health System receives more than a heart-shaped Valentine. The 7-month-old robot, standing 5 feet, 6 inches tall, also receives a name: Dr. Bear Bot.
After a 21-day voting period, 185 children and staff voted on Dr. Bear Bot, which received 36 votes, beating 14 other child-selected names, including SMARTy (Special Medical Access to Remote Technology), Dr. Bot and Rosie, which were submitted during the hospital’s Race for Every Child 5K race and fun walk on Oct. 20, 2018. The news was announced Valentine’s Day to more than 220 patients over WPAW, the children hospital’s closed-circuit television and radio station.
Wi-Fi-enabled robot left the cardiac ICU, often referred to as the tele-cardiac ICU, for the first time since it arrived in late August to attend the robot-reveal party, hosted by Children’s National radio hosts DJ Morgz and DJ Curly Cue. The DJ’s partnered with local nurses and doctors to livestream the interview during the 10 a.m. show.
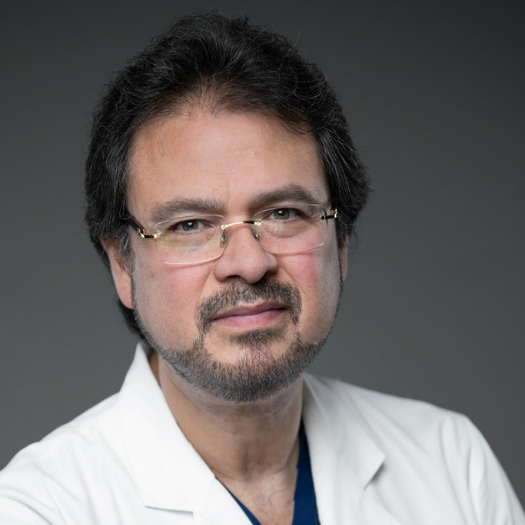
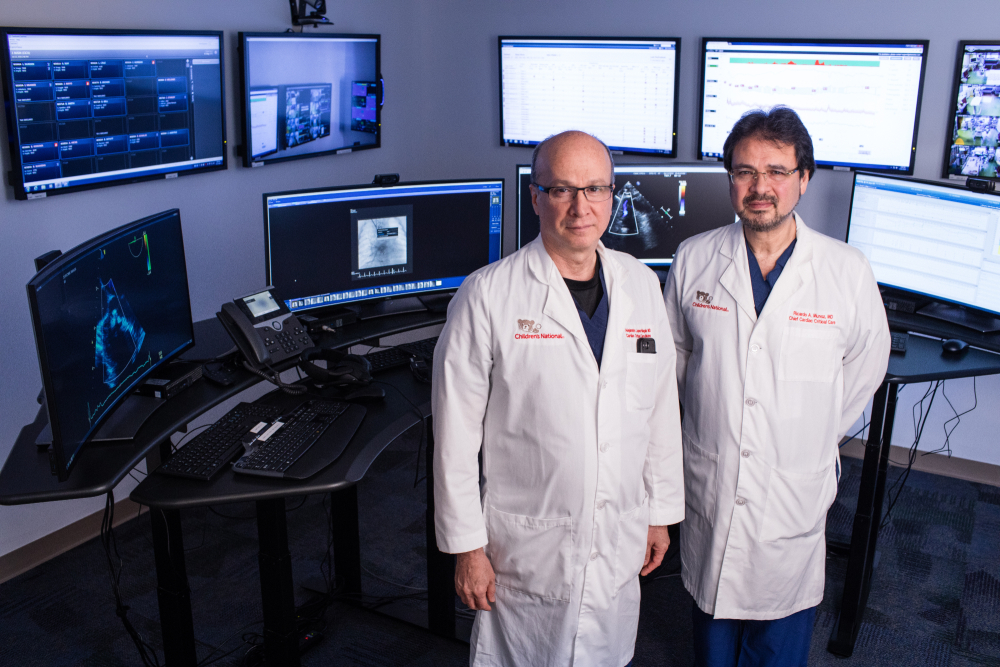
Dr. Bear Bot completed a 90-day test period in the tele-cardiac ICU at Children’s National, which started in September, and the bot now works as a virtual liaison to connect patients, attending nurses and physicians with Ricardo Munoz, M.D., executive director of the telemedicine program and the division chief of critical cardiac care, and Alejandro Lopez-Magallon, M.D., a cardiologist and the associate medical director of the telemedicine program.
Dr. Munoz and Dr. Lopez-Magallon use a nine-screen virtual command center to monitor patient vitals—such as heart rate, body temperature or respiration rate—especially for infants and children who are recovering from congenital heart surgery, flown in for an emergency diagnostic procedure, such as a catheterization, or who are in the process of receiving a heart or kidney transplant. Instead of traveling to individual rooms to check in on the status of one patient, the doctors can now monitor multiple patients simultaneously.
If Drs. Munoz or Lopez-Magallon want to take an X-ray or further examine a patient, they turn Dr. Bear Bot on, drive the robot from its ‘robot-only’ parking space, adjacent to the nurse’s station, and connect with attending doctors and nurses in the teaming area. The onsite clinicians accompany one of the telemedicine doctors, both of whom remain in the command center but appear virtually on the robot’s display screen, to the patient’s room to capture additional medical information and to connect with patients and their parents.
Over time the telemedicine team will measure models of efficiency in the tele-cardiac ICU, such as through-put, how fast a patient checks in and out of the hospital, as well as standards of safety, quality and care, measured by quality of life and short-and long-term patient health outcomes.
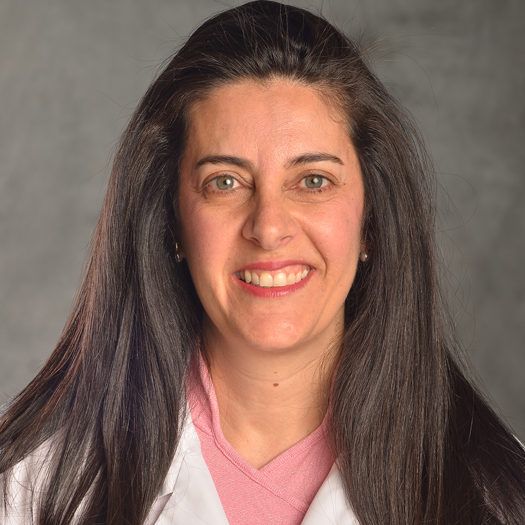
“As technology and medicine advance, so do our models of telemedicine, which we call virtual care,” says Shireen Atabaki, M.D., M.P.H., an emergency medicine physician at Children’s National, who manages an ambulatory virtual health program, which enables patients to use virtual health platforms to connect with doctors, but from the comfort of their home. “We find the patient-centered platforms and this new technology saves families’ time and we’re looking forward to studying internal models to see how this can help our doctors, enabling us to do even more.”
The ongoing virtual connection program that Dr. Atabaki references launched in spring 2016 and has enabled 900 children to connect to a doctor from a computer, tablet or smart phone, which has saved families 1,600 driving hours and more than 41,000 miles over a two-year period. Through this program, virtual care is provided to children in our region by 20 subspecialists, including cardiologists, dermatologists, neurologists, urgent care doctors, geneticists, gastroenterologists and endocrinologists.
To extend the benefits of virtual communication, while saving mileage and time, Dr. Atabaki and the telemedicine team at Children’s National will partner with K-12 school systems, local hospitals and health centers and global health systems.
Meanwhile, Dr. Bear Bot, developed by InTouch Health, returned to a more pressing matter after the robot-reveal party: handing out robot-themed Valentine’s Day cards.
Dr. Bear Bot has an indefinite life span but requires six hours of rest, or full charging, each night. After early-morning rounds with doctors, powering through congenital heart disease trivia in the WPAW studio and handing out Valentines to patients, the tele-cardiac ICU catalyst was ready to recharge.
Media contact: Jessica Frost | 301-244-6721| 202-476-4500