- For Providers
- Colorectal Quiz Podcast
- What You Need to Know About Diagnosing Cloaca
- What You Need to Know About Diagnosing Pediatric Functional Constipation
- What You Need to Know About Functional Constipation and Fecal Incontinence
- What You Need to Know About Medical Treatment for Pediatric Chronic Constipation and Fecal Incontinence
- For Providers
- Colorectal Quiz Podcast
- What You Need to Know About Diagnosing Cloaca
- What You Need to Know About Diagnosing Pediatric Functional Constipation
- What You Need to Know About Functional Constipation and Fecal Incontinence
- What You Need to Know About Medical Treatment for Pediatric Chronic Constipation and Fecal Incontinence
- What You Need to Know About Surgical Treatment for Children With Functional Constipation
- Treatment Options for Cloaca
- Current Treatment Options for Children with Hirschsprung Disease
- Treating Children with Persistent Symptoms After Surgery for Hirschsprung Disease
What is the role of a pediatric surgeon in the management of functional constipation and fecal incontinence?
Pediatric surgeons are often consulted by pediatricians, emergency physicians or pediatric gastroenterologists to assist treating children with severe cases of constipation, fecal impaction and fecal incontinence. Pediatric surgeons perform the following procedures that help improve these conditions:
- Antegrade continence enema (ACE) procedure, also called a Malone appendicostomy
- Cecostomy
- Neo-appendicostomy
- Colon resection
ACE Procedure/Malone Appendicostomy
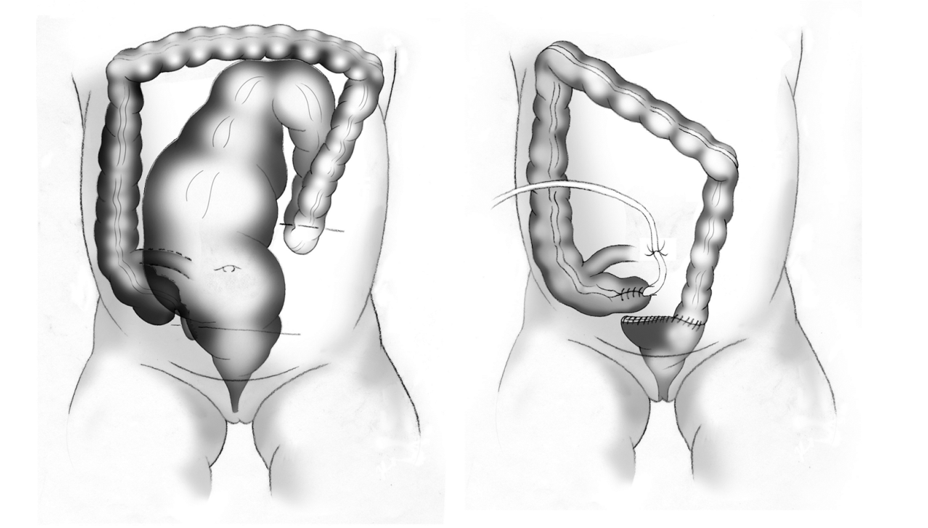
An antegrade continence enema (ACE) procedure, also known as a Malone procedure, is a surgical procedure that involves constructing a tube from the appendix through the belly button through which an enema can be given. This provides an alternative route for the enema, and can more easily be performed by the patient, promoting their independence.
This operation is usually recommended for patients who are capable of being more independent, as it allows the administration of the enema without parental assistance. It should ideally be performed in patients for whom bowel management has been successful. However, for children who cannot tolerate rectal enemas, this procedure is also beneficial as a bridge to continence, enabling the training of the sphincter muscles while the patient tries to hold onto the flush.
Malone Appendicostomy Procedure:
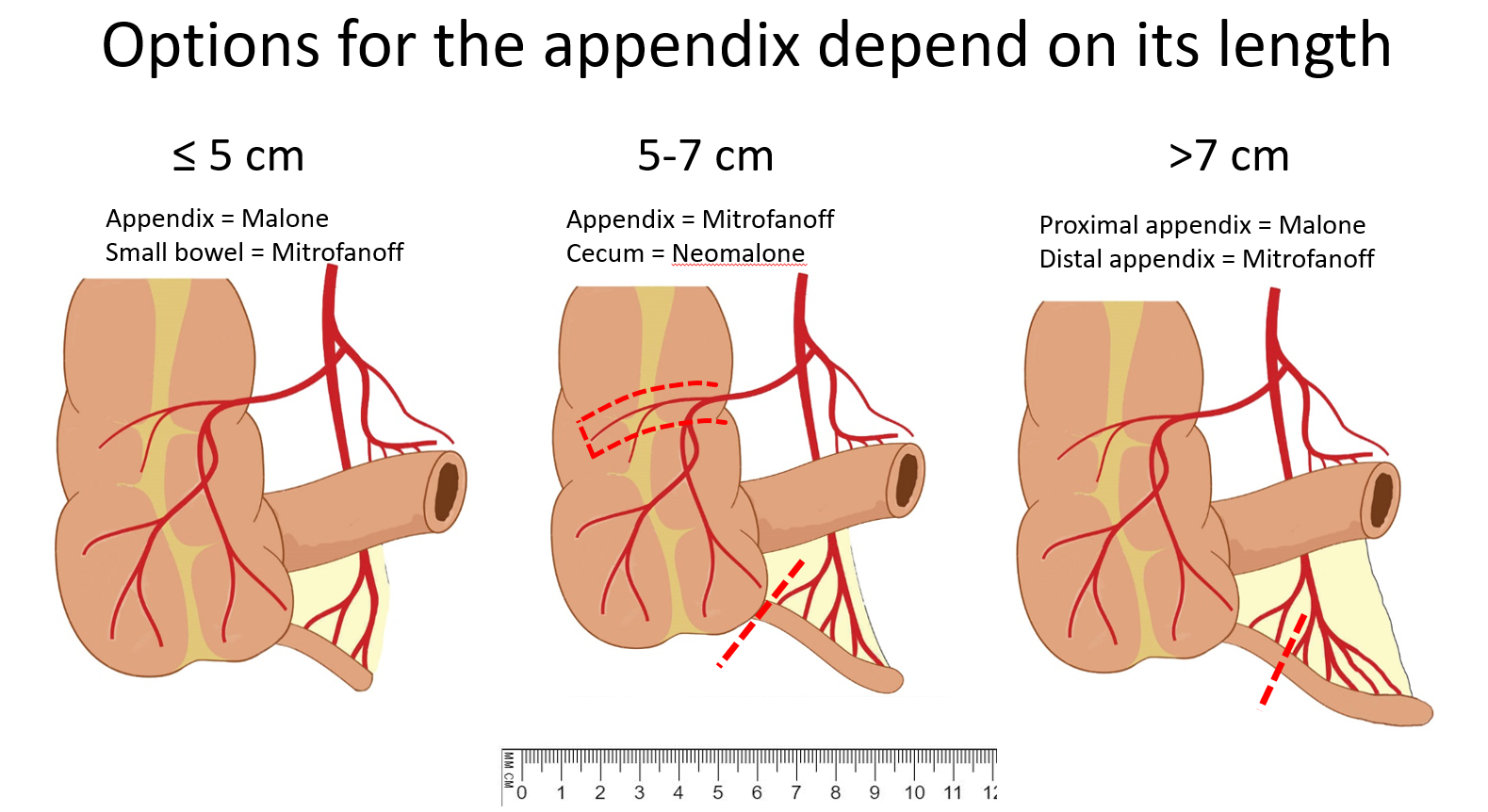
In patients in whom both a Malone appendicostomy and a similar tube construction for the bladder and urinary system are needed, there are various strategies that may be employed to share the appendix, which depends on whether the appendix is a certain length:
Neo-appendicostomy
Cecostomy
In a cecostomy, the healthcare provider puts a tube (catheter) into the large intestines (cecum) located in the lower right abdomen, also for access to place an enema used to empty the colon.
Sometimes “skin-level” devices which are soft, flexible, non-latex tubes, similar to a gastrostomy feeding tube are used. These tubes may be placed through the abdominal wall directly into the cecum using minimally invasive techniques. The benefits of a skin-level device include the avoidance of daily catheterization and elimination of certain risks. This option is ideal for children with sensory processing disorders in whom intermittent catherization is impractical.
When should a colon resection be performed to treat functional constipation?
What are typical outcomes for children who have gone through a bowel management program?
Regardless of the underlying disorder, bowel management plans often require modification over time. Careful follow-up is a key component to a successful program. Specialists caring for children with severe constipation or fecal incontinence must be committed to finding the right program that works for the individual.




